The Top Ten Challenges for ED Security in 2016 and Beyond
The emergency department (ED) is a high-volume traffic area where different situations can arise daily. There are ways to protect your ED and staff, starting with taking a close look at your security program. The ED is one of the most challenging and stressful areas in a hospital where dramatic life-and-death cases can occur at any moment. Following are the top 10 challenges for emergency department security in 2016 and beyond.
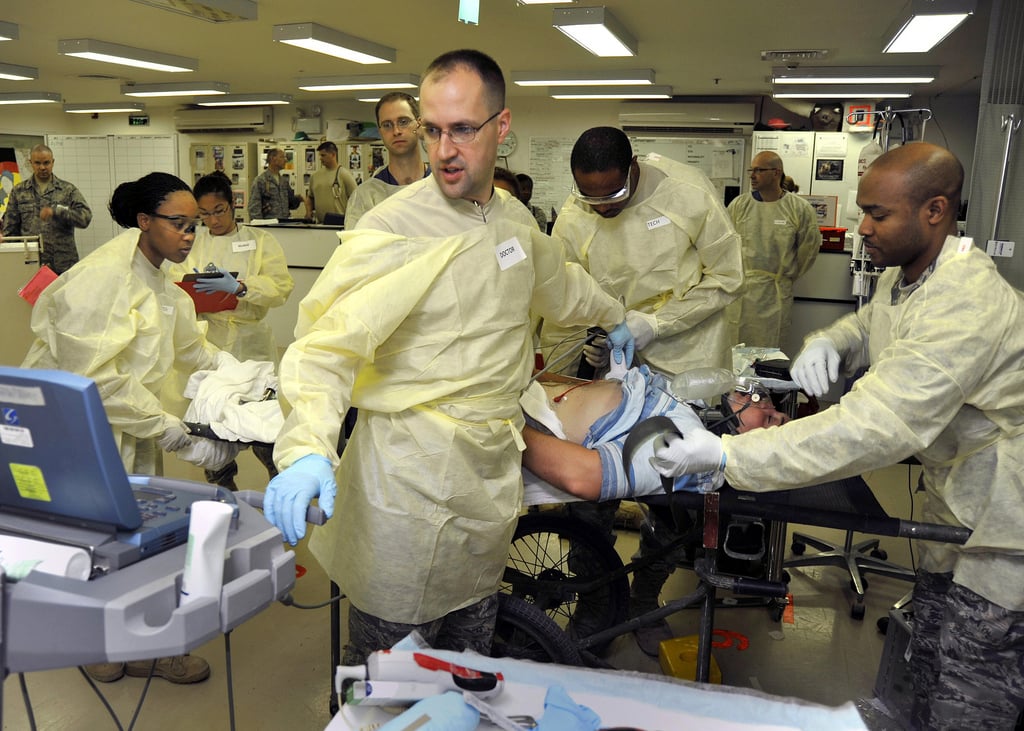
1) Workplace Violence – The Emergency Department Violence Surveillance Study by the Emergency Nurses Association, which surveyed more than 7,000 emergency department nurses, found that the emergency department is a particularly vulnerable place for workplace violence. In the survey, 25 percent of the respondents reported having experienced physical violence more than 20 times in the past three years, and nearly 20 percent reported experiencing verbal abuse more than 200 times during the same time period.
Nurses, as well as doctors and other medical professionals, are on the emergency department’s front lines, facing potentially volatile situations. As reported in Potential: Workplace Violence Prevention and Your Organizational Success, in “inner-city areas, the ED will often get gunshot cases following gang violence episodes, with friends and family members of the wounded following them into the facility.”
Drug and alcohol-induced violence are also common in the emergency department. Domestic violence plays out there as well, with the aggressor following the injured partner to the hospital and attempting to keep them silent on the cause of the injuries.
The Joint Commission, which accredits and certifies U.S. healthcare organizations, has classified the ED as a sensitive area, noting that hospitals and emergency care facilities must have a well-defined security plan to address violence. The plan should include all ED staff, management, human resources, security, and local law enforcement. A comprehensive assessment of the ED’s safety and security plan should be executed often to identify strengths and uncover areas for improvement.
2) The Metal Detector Debate – Hospital administrators and security leaders have a lot to consider when contemplating the use of metal detectors in the ED. The perception of metal detectors in the ED is often debated as it is critical for the community to consider the ED a safe place. The installation of metal detectors may result in some people saying that their very presence implies their community is dangerous. But this type of proactive access control procedure can also be seen as positive security function.
Another consideration is how effective metal detectors are. Using metal detectors in one location, such as the ED, while other entrances are not similarly monitored, defeats the purpose of the metal detector and provides a false sense of security. There must be strict procedures for confiscated items and use of handheld devices to supplement the walk-through device. In addition, training and maintaining the equipment will need to be addressed.
3) Armed Security Considerations – When hospitals evaluate their local crime statistics and review their security programs, they sometimes consider the deployment of armed security officers. Making a decision about the use of firearms or other weapons requires careful consideration of multiple factors including training, supervision, liability, and community response. The decision is not only highly sensitive but also dependent on the needs and culture of the individual facility. There is not an industry-wide recommendation on armed security officers–it must be an individual, facility-specific decision.
Before incorporating firearms into the hospital environment, other tools such as Taser or pepper foam should be carefully evaluated, data and trends analyzed, and a review team formed to help ensure that all factors are considered and the needs of all stakeholders evaluated.
4) Staffing Patient Watch Programs – Patient watch is not to be confused with a “sitter program” where a healthcare attendant watches a patient who is elderly, disabled, or impaired and may be at risk of falling or other non-violent risks. A patient watch is implemented to monitor a patient to protect that patient and others from violent or aggressive behavior. The patient must be identified, as per the laws of the individual state, as a threat to themselves or others and placed in an involuntary patient status by the appropriate authority, which could be law enforcement or clinical staff.
Well-trained security officers are an excellent resource for patient watches. While medical and security staff must collaborate, the clinical demands of medical staff often prohibit them from being assigned to conduct patient watches. Ensuring the appropriate staffing is the number one priority for effective patient watches. Will a security officer be pulled off their regular post to be assigned to patient watch? Will someone be assigned from outside the organization? Are dedicated patient watch security officers assigned to each shift? If a patient is aggressive and a security officer is responding, back-up security needs to be close at hand. Also, because an aggressive patient is susceptible to adverse health developments, it’s critical that medical staff are prepared to respond quickly.
5) Maintaining Crowd Control – A number of extenuating circumstances, from a high-profile shooting victim to an outbreak of the avian flu, can rapidly transform a quiet ED into a very crowded place. Situation-specific protocol needs to be established. For example, the shooting of a police officer will attract scores of media and law enforcement. Protocol for this situation often includes establishing staging areas outside of the ED for the media and police to convene. In the event of a major flu epidemic, a triage area could be set up to address urgently sick patients, isolating these highly contagious people from the rest of the ED population. Advanced identification of potential situations and the development of corresponding plans will allow for seamless response and minimized disruption to hospital operations.
6) Social Media and Patient Privacy – The use of social media by medical institutions has increased dramatically and has proven to be an efficient means of sharing information and communication with the community. However, employee social media use while on duty can pose a risk. Anyone who works in the medical environment is just a tweet or Instagram post away from violating federal patient privacy requirements. Health Insurance Portability and Accountability Act (HIPAA) maintains stringent patient privacy standards for everyone who works in the medical field, from doctors, nurses, and administrators to security officers. It is important for all medical facilities to have formal social media policies with clear guidelines on appropriate social media usage and the repercussions for violating them.
7) Security Awareness Training for ED Staff – Training for the ED staff, beyond what’s prescribed for a healthcare profession, is vital so they can learn to recognize abnormal behavior and know how to diffuse a violent situation. Staff need to be confident in the plan and understand the major role they play in keeping the ED safe. Make sure that your staff understands that violence against them is never appropriate and establish reporting procedures. A culture of collaboration will help medical and security staff work together, and shared training will foster team work.
8) ED Security Team Training – It is generally understood that training is an essential part of an effective healthcare security program, but how much training is necessary? What if a security officer already has experience? The importance of relevant and ongoing training for security officers working in healthcare facilities cannot be overstated. It is critical to ensuring the safety and security of a hospital’s staff, patients, and visitors.
Even if a security officer who is new to a facility has previous security experience, or worked in a similar field such as law enforcement, training is still critical. Every healthcare facility is different and security officers must receive the appropriate training. There are three primary categories of training in healthcare security:
Basic Security Officer Training – Security officers must complete training in standard security procedures such as patrolling, report writing, and access control; as well as training appropriate to their assigned duties. For example, those serving in an ambassador capacity should receive enhanced customer service training.
Industry-specific Training – Healthcare security officers must also be trained in state and federal regulations and standards, HIPAA, and infection control. The security team needs training to understand and support the hospital’s compliance efforts. For example, a well-trained security officer who understands the essentials of HIPAA regulations sees a box of discarded papers containing protected health information (PHI) near the trash dumpster and immediately reports it to hospital administration, potentially avoiding fines and/or a loss of accreditation for accidental disclosure. Or, if a visitor is asked to leave the hospital for disruptive behavior and later returns seeking emergency medical treatment, a security officer who is aware of the Emergency Medical Treatment & Labor Act knows that this person cannot be turned away, as that would be a violation of federal law.
Hospital-specific Training– Even if security officers are up-to-date on the previous two categories, they must receive training pertinent to the facility. Department-specific codes and procedures can vary by hospital, as will access control and incident reporting processes.
9) Emergency Preparedness Planning – The need for comprehensive emergency preparedness plans in a hospital cannot be overstated. And, establishing a plan that addresses patient, staff and visitor safety–in a range of emergency scenarios–is only the beginning. Ongoing communication, training and drills are critical for the entire facility and especially the ED with its constant flow of people in various medical states. Being unprepared for, or unable to seamlessly respond to an emergency, can create serious concerns if security personnel are therefore unavailable to manage access control, aid distressed patients and otherwise secure the facility as usual. The most effective emergency plans are comprehensive and incorporate the security team who will lead these plans when activated.
10) Delivering Customer Service through Security – Security personnel are highly visible and strategically positioned to interact with all individuals entering the ED. With proper training, the security team can become a valuable part of the effort to create a positive patient and visitor experience. If they see someone getting emotional, a well-trained officer will immediately step in to try and calm them down before the situation gets out of control. They may offer the person a coffee or blanket, or simply a friendly ear.
Part of creating an outstanding ED experience includes producing and maintaining a safe, secure and customer-friendly environment for patients, visitors, and staff. Security officers can take on a customer service role—by combining customer service and security, visitors, patients, and staff feel safe and engaged.
In an industry as dynamic as healthcare, it’s easy to move existing programs that seem “good enough” to the back burner to focus on more pressing and urgent needs. Even if an ED has already implemented changes to its security program, periodic assessments should be performed to ensure that it remains effective. Regularly evaluating and improving the security program will help keep the ED’s staff, patients, and visitors safer, and will contribute to a more positive atmosphere for the entire facility.
--
Kenneth Bukowski is Vice President, Vertical Markets, at Allied Universal and can be reached at [email protected].